I haven't written for this blog in a long, long time. Looks like most of my thoughts are on the "naughty" side now. Even so, I wrote this post for my naughty blog back in January and thought I would share it here as well. I'm finally getting back to writing but it's taken almost 7 months. I'm not sure whether it was fear that was holding me back or uncertainty. But I'm taking a chance and writing again. As a further note, he is doing so much better now. His voice never fully recovered, but mentally and physically he's back to full strength.
One of the most emotionally complex and difficult things a person can experience is taking care of an ill or elderly spouse or parent. When my husband became critically ill, my world turned upside down. I'm a fairly strong person, but there were times when I feared ever getting him back, and I'll admit I lost hope.
As I searched through the Internet looking up conditions and treatments, I discovered that having my normally dominant husband growing totally dependent on others for his health and welfare was similar to caring for an elderly parent. The difference being that my husband always held the potential to get well again while an elderly parent cannot grow younger.

The shock of having him laughing and joking with me one minute, then sedated, unconscious and on life support the next was almost my undoing. Since I was told he could still hear me, though he most likely wouldn't remember anything because the sedation they had him on also affected memory, I would sit beside him and carry on conversations. I liked to be with him whenever they did what they called a "sedation vacation" where they took him off sedation to see if he could follow simple instructions like opening his hands, grasping fingers and wiggling his toes. In the beginning, these commands appeared to be fairly easy for him to carry out, but the longer he remained sedated and on the ventilator the more difficult it became for him to respond.
I had great difficulty accepting the changes occurring in him. He was the stronger one and he took care of me, now it was my responsibility to take care of him. To make sure his needs were being met both medically and therapeutically.
Since he was unconscious the first few weeks of his hospitalization, I was attempting to keep my head up while I frantically tread in uncharted waters. I took things one day at a time, celebrating every small victory, and trying not to lose hope when his progress appeared to be taking a backward turn. The most difficult day for me was when we first attempted to take him off the ventilator. I expected him to be groggy and a little out of it, but still pretty much himself. He sat with his mouth open and tongue hanging down to one side as he struggled for every breath he took. I watched as his oxygen levels slowly sank into the 70s while his CO2 levels rose into the 90s. His eyes were so vacant and glazed, I doubt he even recognized me. He would only breathe through his mouth, but by the time they attempted to put a BiPap mask on him, his stats indicated he had to go back on the ventilator and quickly. I cried then. Not because he had to be ventilated again, but because even though his body was right before me, nobody was home and I was afraid he was forever lost to me.
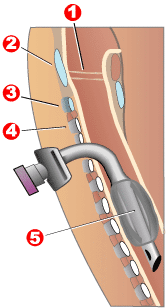
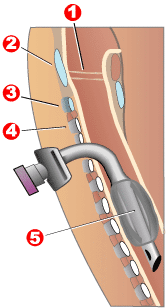
After another week on the ventilator, I agreed to having them perform a tracheotomy, He could still be on the ventilator with a trach, but they could take him off sedation, which would allow him to interact more with his caretakers. I was told the stoma and trach didn't need to be permanent, but given his last reaction to being taken off ventilation, I suspected he would require assistance, at least at night, for the rest of his life. However, he'd never get stronger while he remained unconscious and there was a chance he'd eventually improve if he could move around, and engage more with his surroundings.
The nurses and speech therapist talked to me then about ICU delirium, which when you read about it can be pretty terrifying. As I look back now, I'm pretty sure he suffered from it along with his other problems. His apparent cognitive impairment once he was off sedation was severe. In some ways he reverted to the mentality of a two-year-old. His behavior was impulsive and he liked touching different textures (blankets, sheets, whatever he could reach). He could follow simple commands (grip hands, move legs), but had great difficulty making any sort of assessment (cold, warm, discomfort, etc.). He lost track of time and where he was, even whether it was day or night despite the large window in his room. He couldn't maintain focus for longer than a few seconds. Even when he could do these things, and appeared to be able to hold a conversation, he wasn't fully comprehending what he was saying. He was making what he believed to be an appropriate response without really understanding.
None of this surprised me after their first attempt at extubating him, and as he steadily improved, I praised his small successes. What I didn't expect was the total personality change that overcame him. The nurses claimed he was sundowning, but the differences in him appeared much worse than that. He would physically resist his caretakers and even attempted to bite a couple of nurses when they reached out to secure his nasogastric tube. He eventually yanked out the feeding tube himself despite receiving many instructions to leave it alone. He'd both challenge and insult the doctors as he grew more and more paranoid, telling me that everyone in the hospital wanted to keep him sick in order to get more money. He was convinced they were secretly trying to hurt him. I knew his fears weren't rational, but I acknowledged them as I did my best to assure him that everyone caring for him was there to help. I even had the nurse call up hospital security in attempt to assure him there were people he could call on if he was in trouble and they would protect him. He appeared to accept what was he was told, but I knew he wasn't convinced. Everyone, except me, was in collusion to steal his hard-earned money.
In his efforts to leave the hospital, he yanked out four trachs in a period of two days. By Sunday, Respiratory had no more of his size in their stock, and the stock room was closed. So, if he pulled out his current trach, we would have a medical emergency. To be sure he couldn't, they kept him in soft restraints when I wasn't there.
Another thing I didn't expect was his anger with me. But since he has no recollection of how difficult he was being, his behavior was clearly part of the delirium he was suffering. I tried to give him options and choices. In the beginning nothing interested him, but as he slowly became more aware of his surroundings he showed a modicum of interest by selecting the television programs he normally watched. However, he still had difficulty ascertaining night from day, and would insist there should be a football game on Thursday morning. When he couldn't find it after switching through all the channels, he became convinced the hospital was censoring his television. Eventually, this too passed as his comprehension and awareness grew. But with this success came another backward spiral when he refused to work with his therapists, resisting their instructions and insisting they should just let him leave the hospital. He grew convinced he was just fine when in reality he couldn't even sit up by himself. However, he did want to use the bathroom rather than a bedpan. I told him if he ever wanted to use the bathroom again he needed to at least try to do as his therapists asked. So, he grudgingly participated in the beginning, but as he physically improved, so did his attitude until he finally took an active part in his therapy.

Even the therapists were amazed by his daily improvements. However, in addition to the problems I faced with his recovery, I was battling our insurance company. They kept refusing to send him places that were equipped to deal with the different stages of his recovery, so the ICU became his acute therapy unit. Everyone in contact with him worked to get him up and moving. Eventually, he was taken off the ventilator and equipped with a speaking valve on his trach, and finally off the trach itself until all he had was an oxygen cannula for support. At that point he no longer needed to be in the ICU and was moved to a regular room in the hospital. However, he stayed in the ICU for 34 days and was in the hospital for a combined total of 38 days before they moved him to a skilled nursing rehabilitation facility where he spent his birthday, Christmas and New Years. The holidays interfered with his therapy, so when the therapists weren't available to work with him, I convinced him to get up and walk the hallway at the very least while I followed him with his oxygen canister. He continued to improve both physically and mentally so quickly, he was released from the facility after only 16 days and no longer required oxygen support.
Though we still have no definitive answer as to what caused his problems, I've got him home now. He still has difficulty with his balance and walking, but he doesn't require a walker in the house. Though he's no longer on oxygen, I purchased an oximeter and we measure his oxygen at least twice a day. It's usually around 98, which is where he was before all this happened. We now have a nurse as well as three therapists who visit him a couple of times a week. He is beginning to take control of his life again. We even went grocery shopping together, and he rode one of the electric carts while I followed and collected the things he couldn't reach.

He is back to working at his computer, and is getting stronger every day, although his voice is still a little rough from his multiple intubations. All in all, I'd say he was a success story. I bought him a fitness bracelet and we are monitoring his sodium intake as well as his weight to make sure the swelling in his legs continues to go down. Thanks to all who sent me well-wishes. I hope to get back to writing and social media in a few weeks. Right now, he continues to be my priority.